Every single day, RiverSpring Living—a post-acute and long-term care provider—ensures around 18,000 New Yorkers have access to the highest-quality services that the healthcare sector can offer.
This includes a 600-bed skilled nursing complex, numerous assisted and independent living facilities, and home care agencies – where visiting nurses, therapists and aides are sent to patients’ homes to provide therapy, housekeeping and more.
Founded more than 100 years ago in Harlem, New York, RiverSpring is still looking after some of the most vulnerable members of society.
Look no further than the Weinberg Center, a shelter that brings in elders who have been abused either physically, emotionally, sexually or financially, and gives them access to legal and emotional support.
Another recent project has involved working alongside a real estate developer to build subsidised apartment buildings, where people previously living on the streets or in shelters can be provided housing, support services and essential skills like meal planning, money management and taking care of their own health.
What’s more, RiverSpring’s managed care programme services about 17,000 people, who give up their traditional insurance to join the organisation’s own insurance plan.
This ensures a nurse visits them every six months, doctor’s appointments are fulfilled and necessary medication is received, keeping patients healthy and generally reducing costs associated with the care system.
All told, RiverSpring Living is one of the US’ biggest freestanding not-for-profits specialising in long-term care.
“We're dedicated to helping older adults live the fullest lives they possibly can,” outlines David Finkelstein, CIO at RiverSpring. “We’re transforming the landscape so that we can provide the best care and the best services.”
A rapid evolution
Since Finkelstein joined in 2012, RiverSpring Living has skyrocketed from around US$200m to an astonishing US$1.2bn.
Back then, managed care plans were just getting off the ground and a significant proportion of the supportive housing didn’t even exist. In fact, RiverSpring’s core business proposition was its nursing home in Riverdale, accommodating almost 900 beds.
However, as Finkelstein explains, the organisation has had little option but to evolve to keep pace with rapidly-changing demands.
“What we've been doing is reducing the number of beds in our nursing home because the need is less,” he explains. “People want to live at home or they want to live in alternate settings, as opposed to the nursing home.
“Plus, most of our nursing home residents are under the state Medicaid programme, which hasn't kept pace with reimbursement to our costs, so we lose money every single day for every patient we serve in our Medicaid programme.”
In reality, this means RiverSpring has been forced to pivot into other business lines to balance the books and survive, offsetting the losses being suffered at the nursing home with the surpluses earned from other areas.
Luxury independent living
RiverSpring’s immense growth is perhaps best demonstrated by its plan for a state-of-the-art facility called River’s Edge.
Situated on a stunning, 32-acre campus by the Hudson River and just minutes from Manhattan, River’s Edge is what’s known as a continuing care retirement community, offering independent living with an insurance product wrapped around it.
The concept is that prospective residents pay an entry fee—some of which may be refundable, some of which may be amortised depending on their plan—to secure a luxury apartment at a new 260-unit, 11-story building which is currently being designed.
One thing’s for sure: this certainly won’t be your average retirement facility. RiverSpring’s goal is to offer a Ritz-Carlton level of amenities, including a saltwater lap pool, yoga and Pilates studios, a golf simulator, tennis courts and no fewer than three dining venues.
“The whole idea is that residents are in a building with seniors of their age, so they have community,” Finkelstein continues. “They'll have activities that they can attend and we’re actually located directly next to the University of Mount Saint Vincent, meaning they’ll be able to audit and take classes for a continuing education.
“We’re a 20-minute drive away from Manhattan, so they can go to Broadway and see a show, or go to a restaurant.”
Of course, the huge healthcare benefit to all of this is that, while River’s Edge offers independent living, residents are entitled to care services for the rest of their lives, whether it be a shift to assisted living, short-term rehabilitation or something more complex.
It’s all part of the insurance-apartment concept offered by RiverSpring.
“As a resident’s health declines over time they may not be able to live independently in their apartment, so they can move to our assisted living building for the same fee,” adds Finkelstein. “And, as their health declines towards end-of-life, they can come into the nursing home.
“We have a longitudinal record, so we know each resident’s likes and dislikes, how they work, their medications and medical history, so we can treat them better and help them for the rest of their lives.”
Harnessing the power of AI and robotics
Clearly, it would be remiss of RiverSpring Living—not to mention its technology function—to neglect considering how groundbreaking technologies like AI, machine learning and robotics can be used to improve operations and, most importantly, patient care.
Finkelstein is keen to mention that, when the company first embarked on its digital transformation journey, a conscious decision was made to hire a full-time project manager with a nursing background to ensure technological advancements are embedded and incorporated into day-to-day operations.
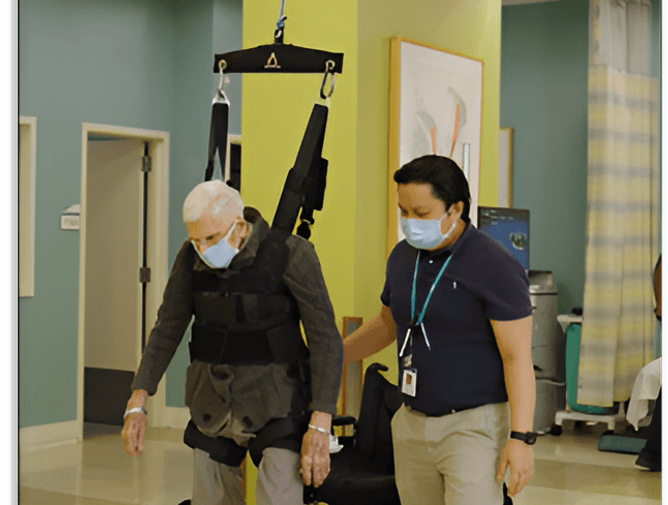
Proof of this can be seen in a project aimed at reducing rehabilitation time among residents following major surgery, such as a knee or hip replacement, which harnesses AI-powered robotics.
Working alongside a company called Aretech, RiverSpring has installed a ZeroG robot that runs on a track attached to the ceiling in its rehabilitation gym and supports the patient using a harness, taking up to 60% of their body weight.
“Before this, we’d have two therapists holding the resident by their waist, helping them to ambulate and essentially learn how to walk again,” details Finkelstein. “But the robot is smart enough to know when they’re going to fall and will pull them back up.
“Not only does it save the resident from falling, but gives them the confidence to push further than they normally would.
“We’ve proven this can help patients recover faster. We can return people to their previous level of function within 21 days, whereas it used to take 28, plus we’ve made them stronger and more confident.”
Another innovation worthy of mention is an AI-powered service called VirtuSense, a sensor-based system installed in the rooms of patients at risk of falling.
“Sometimes, when people come into a facility, they're a little disoriented,” Finkelstein goes on. “It’s the same after some types of surgeries or even medications, so getting out of bed and falling is a big risk.
“These sensors passively monitor the resident and, anytime it senses motion that indicates they're trying to get out of bed, it will alert nurses to go to the patient. In the rooms, it will announce in a soft voice, ‘Please stay in bed, wait for the nurse to come’.”
The result has been a 25% reduction in falls in units where VirtuSense has been piloted, with the potential for this to rise given the sensors are constantly learning about the typical movements of each patient.
Finkelstein adds: “By keeping people safe in their rooms, it’s prevented a lot of hospitalisations and saved lives.”
Embracing VR
RiverSpring began embracing virtual reality (VR) about three years ago in a bid to ease patient isolation – a big problem in the care sector and among the older generation in general.
The more conventional form of VR, where users can put on a headset and be transported to a place of their choosing, has worked wonders in combatting isolation.
“Some residents like to enter a street address so they can see where they grew up or went on vacation and reminisce, which brings up a lot of good memories,” says Finkelstein.
Elsewhere, RiverSpring has purchased several GoPro cameras so that family members can film events like weddings, birthday parties or a grandchild’s big game, ready for the footage to be uploaded onto a headset for residents to experience and enjoy from the comfort of their own accommodation.
These GoPros are also coming in handy for the rehabilitation and discharge process, especially when patients go to RiverSpring for care following major surgery, before heading back home.
Cameras are again loaned to family members who are encouraged to film the patient’s living quarters, allowing RiverSpring to carry out a virtual walkthrough, point out potential hazards or obstacles and make any necessary adjustments.
Finally, residents and family members are using VR headsets to meet in a virtual environment, where their avatars can talk and interact as if they were together.
“We're doing that now with a number of our more alert residents,” Finkelstein continues, “and it’s been a very good learning experience.”
Partnerships accelerate digital transformation
Two projects in particular went “full throttle”, as Finkelstein puts it, at the very beginning of RiverSpring Living’s digital transformation.
The CIO pauses here to pay tribute to the Hauser Foundation, which left a generous gift to thank staff members for the care extended to Gustave Hauser, a patient at RiverSpring during the COVID-19 pandemic.
“Rita Hauser has been very thankful for the service we provided to her husband and gave us a sizeable donation to be used only for technology projects,” Finkelstein explains. “So, that was the springboard that allowed us to think bigger than our budgets.”
The first project of note highlighted by Finkelstein is an investment in automated vital signs carts, in this case provided by Medline and seldom seen in long-term care facilities.
It means all vital signs can be recorded simultaneously and automatically entered into electronic medical records, saving nurses an estimated four to six hours per week due to no longer having to do this manually, and allowing them to instead focus on patients.
Meanwhile, Finkelstein reveals one of the biggest concerns held by residents, families and care organisations across the sector is having slow response times.
RiverSpring had already worked with Unimed over the preceding couple of decades to install traditional nurse call systems but, deciding the time was right to upgrade, the firm issued an RFP and ultimately selected Ascom as its solution of choice.
Now, when a resident presses their nurse call button, an alert is immediately sent to mobile phones carried by staff members, allowing them to triage the numerous calls they receive and take whatever action is required.
As it stands, the goal is to answer calls within three minutes, and, during the system’s first year in place, the average response time for more than 100,000 calls stood at one minute and 55 seconds.
“Partnerships are critical, and both Unimed and Ascom have been amazing partners,” concludes Finkelstein.
“We really don't want to have a transactional relationship with our vendors. We want to know that, if we have a problem, they're going to be there to support us. And if they need a reference or some recommendations from their manufacturers to help redesign a system, they know they can come to us for guidance.
“Our partners are the ones helping us become successful, so we really look at partnerships as a two-way street.”
Make sure you check out the latest edition of Technology Magazine and also sign up to our global conference series - Tech & AI LIVE 2024
**************
Technology Magazine is a BizClik brand



- OpenText AI: Empowering Businesses in Information ManagementDigital Transformation
- RiverSpring Living, Ascom and Unimed Transform Senior LivingEnterprise IT
- RiverSpring Living, Ascom and Unimed Transform Senior LivingDigital Transformation
- Inside RiverSpring Living’s Remarkable TransformationDigital Transformation